|
|
Pulmonary Arteriovenous Malformations
AVM
General Considerations
- Defect in capillary structure
- Usually congenital in origin
- Cirrhosis
- Cancer
- Trauma
- Surgery
- Actinomycosis
- Schistosomiasis
- Hemangioma of cavernous type
- Age
- 3rd–4th decade
- Mostly manifest in adult life
- 10% in childhood
- Simple type (80%)
- Single feeding artery empties into bulbous, nonseptated aneurysmal segment
- Single draining vein
- Complex type (20%)
- Two or more feeding arteries empty into septated, aneurysmal segment
- Two or more draining veins
- Complex types are more frequently in the lingula and right middle lobe
Clinical Findings
- Asymptomatic in most until 3rd or 4th decade if AVM is single and <2cm
- Epistaxis is most common presenting symptom (80%)
- Dyspnea on exertion (60%)
- May also have hemoptysis secondary to rupture into bronchus commonly
- Cyanosis with normal-sized heart (R to L shunt in 25-50%)
- Clubbing
- Bruit over the lesion which > with inspiration
- Orthodexia = increased hypoxemia with PaO2<85 in erect position
- Palpitations, chest pain, no CHF
Imaging Findings
- Location
- About 2/3 in lower lobes
- Then, middle lobe
- Then, upper lobes
- Medial third of lung
- Often subpleural
- Bilateral in about 1/2
- Conventional radiography
- Sharply defined mass (90%)
- Cord-like bands from mass to hilum (feeding artery and draining vein)
- 2/3 single, 1/3 multiple
- Enlarge with advancing age
- Change in size with Valsalva maneuver (decrease)
- Phleboliths (rarely)
- CT
- Study of choice is contrast-enhanced chest CT
- Feeding vessel or vessels
- Rapid enhancement on dynamic CT
- More sensitive than angiography in picking up multiple lesions
Differential Diagnosis
- Other causes of solitary or multiple pulmonary nodule(s)
- Carcinoma of the lung
- Hamartoma, adenoma, granuloma
- Mets
- Wegener's
- Rheumatoid nodules
Treatment
- Embolization of feeding vessels with coils/detachable balloons
Complications
- Osler-Weber-Rendu Syndrome
- Associated with Osler-Weber-Rendu Syndrome (30-88%)=hereditary hemorrhagic telangiectasia
- Only 15% of those with Osler-Weber-Rendu Syndrome have pulmonary AVMs
- Family history with this disease
- Epistaxis common
- Telangiectasia of skin and mucus membrane
- GI bleeding

- TIA
- Stroke
- Cerebral abscess secondary to loss of pulmonary filter function
- Hemothorax 2° rupture of subpleural AVM
- Polycythemia
- Congestive heart failure
Prognosis
- After embolization, show about 96% of AVMs were subsequently undetectable
- 11% mortality

Pulmonary AVM. A 3 dimensional rendering of the lower lungs in the axial plane demonstrates an arteriovenous malformation (black arrow) with an enlarged feeding artery and draining vein (black arrows). The diaphragm is shaded pink.
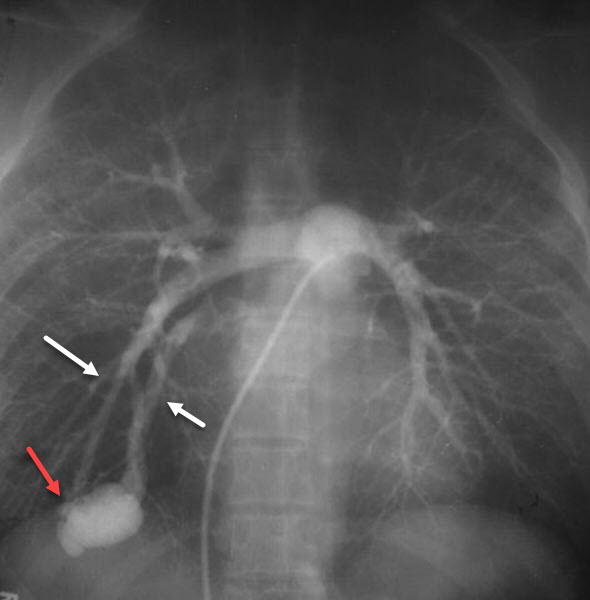
Pulmonary AVM. Contrast-injection via a catheter in the main pulmonary artery fills a lower lobe arteriovenous malformation (red arrow) via single feeding and draining vessels (white arrows).
For more information, click on the link if you see this icon 
|
|
|